Lab-Grown Vaginas: A Leap Forward in Regenerative Medicine

In recent years, the field of regenerative medicine has made remarkable strides in pushing the boundaries of what we once believed was possible. One of the most striking breakthroughs has been the successful growth of personalized vaginas in the laboratory, followed by their implantation into patients.
This avant-garde procedure, which makes use of the patient's own cells, has significant implications for treating a range of medical conditions, from congenital anomalies to the repercussions of cancer or trauma.
The Need for Vaginal Tissue Reconstruction
Vaginal agenesis or the underdevelopment of the vagina is a congenital condition affecting thousands of women worldwide. It presents significant challenges not just physiologically but also psychologically. Traditionally, reconstructive surgeries have used tissues from other parts of the body or synthetic materials. However, both approaches come with complications such as rejection, scarring, or lack of natural function.
Furthermore, vaginal cancer or injuries can result in a significant loss of tissue, further necessitating the need for viable and effective reconstructive strategies. Herein lies the revolutionary potential of lab-grown vaginas.

The Pioneering Process
The methodology behind cultivating a functional vagina in the laboratory is both intricate and fascinating. The foundational step begins with a biopsy: a small piece of vulvar tissue is taken from the patient. This sample, surprisingly smaller than half a postage stamp, is the starting point for a process that will culminate in a fully functional organ.
Once the biopsy is secured, the tissue is disintegrated into its cellular components. These cells, now in isolation, are provided with a nutrient-rich environment, enabling them to multiply exponentially. Within a few weeks, millions of cells are generated from the initial tiny sample.
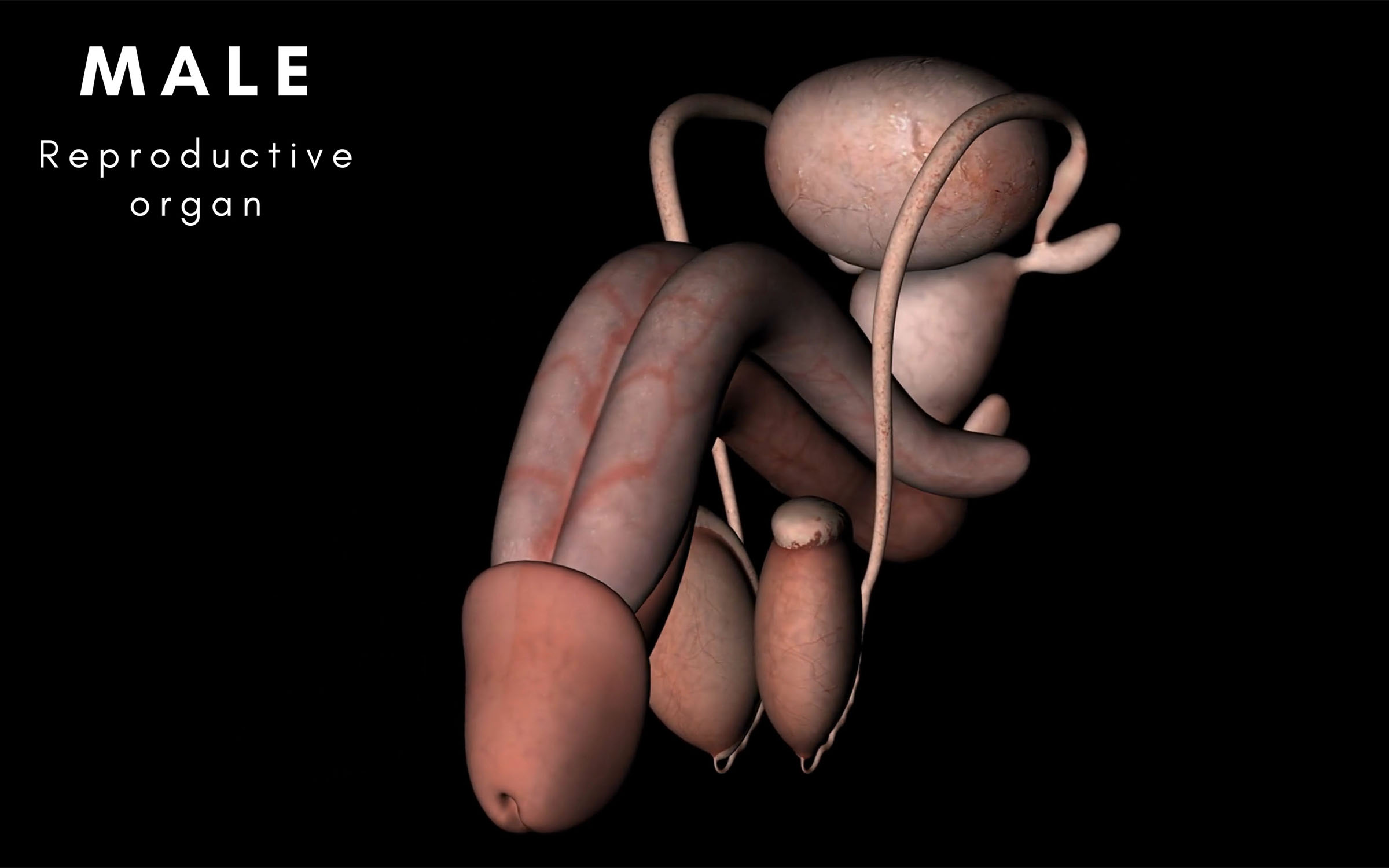
The vagina, in its structural essence, comprises two primary layers: the outer muscular layer and the inner vaginal epithelial layer. The challenge for scientists was to coax these newly grown cells into organizing themselves into these two distinct layers. Their innovative solution came in the form of a biodegradable scaffold, made of a fabric-like material, which acts as a guiding structure for the cells.
The muscle cells are introduced on one side of the scaffold while the epithelial cells are placed on the opposite side. Over time, as the cells proliferate and spread across the scaffold, they naturally differentiate and form layers that closely resemble the natural anatomy of a human vagina.
The process can be tailored to each woman and her special needs for her body type and size. This may lead to having vaginas designed for specific purposes, such as deeper vaginas, tighter or more toned vaginas with additional layers of muscle tissue allowing for more sexual stimulation. But for the current stage, this is a leap forward to have the ability to generate a vagina for patients who truly need one.
The Triumph of Transplantation
After successfully cultivating the vagina in the laboratory, the next pivotal step is transplantation. Given that the organ has been grown from the patient’s own cells, the risk of rejection, a major concern in transplantation medicine, is significantly minimized. Once implanted, the biodegradable scaffold begins to disintegrate, leaving behind a fully functional organ that seamlessly integrates with the patient's body.
Encouragingly, patients who have undergone this procedure have reported satisfactory outcomes, both in terms of the organ's physiological function and its sensation. Many of them are now leading sexually active lives, a testament to the organ's naturalistic function and integration.

The Horizon of Regenerative Medicine
The success of lab-grown vaginas is a beacon of hope in the realm of regenerative medicine. It exemplifies the potential of utilizing a patient’s own cells to address organ defects or injuries, thereby sidestepping complications like rejection or the need for lifelong immunosuppressants.
While the implications for treating vaginal cancer or injuries are evident, this advancement also paves the way for potential solutions to other organ defects or damages. The science behind lab-grown vaginas is not just about the organ itself but stands as a symbol of a future where bespoke organs can be grown in the laboratory, tailored for individual needs, reducing the wait for organ transplants and significantly enhancing the quality of life for countless patients.